Frozen Shoulder
Frozen shoulder is also known as adhesive capsulitis. In adhesive capsulitis, the shoulder joint capsule has adhesions and inflammation. Adhesions are fibrotic bands of scar tissue which joins the surfaces of two anatomic surfaces that limits the motion of the shoulder. This condition is more common in females and the prevalence is more command in diabetics and after the age of 40.
There are several shoulder conditions that cause pain and reduce motion. The primary symptoms of the frozen shoulder are pain and stiffness. Pain may be worse at night and is provoked by laying on the affected shoulder. Normal activity like dressing answering the phone or working will become difficult. Primarily frozen shoulder occurs without an identifiable cause. Frozen shoulder may occur as a result of injury, surgery or illness. People who have suffered from a stroke, thyroid disease (Hyperparathyroidism), inflammation, autoimmune reaction, Parkinson’s disease are more prone to frozen shoulder.
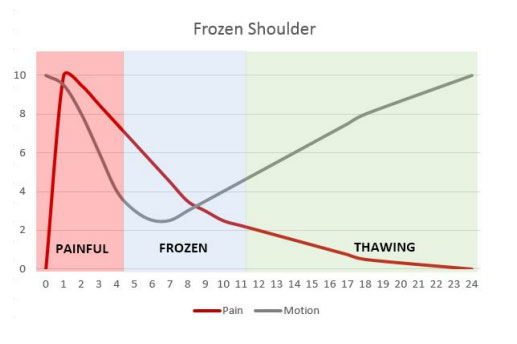
Frozen shoulder has three distinct stages of progression. Each stage typically takes months to progress. The first stage is “Painful Stage”. Shoulder pain is the hallmark of this stage. It starts gradually and progressively worsens. The Second stage is “Frozen Stage” pain may reduce in this stage, although shoulder stiffness and restriction increase. Shoulder range of motion is dramatically reduced. “Thawing Stage” is the third stage. It is characterized by spontaneous thawing. The range of motion will gradually increase and the shoulder will be more responsive to stretching exercise and treatment.
Treatment:
The most common treatments for frozen shoulder are mobility exercise and anti-inflammatory drugs. Manipulation of the shoulder joint is also indicated. In resistant case, injected steroids are utilized.
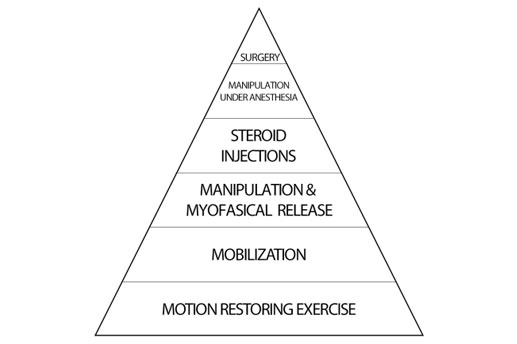
The goal of the manipulation is to manually break free restrictive adhesions and to restore motion.
It is used to free adhesions that limit motion and create pain. Myofascial release is typically a slow stretching of soft tissue that is performed while applying a sustained pressure to the connective tissue of the involved structures.
When more conservative measures do not work, more intrusive treatment can be employed. These interventions include steroidal injections, manipulation under anaesthesia (MUA) and surgery.
- In MUA, the patient is sedated to reduce the level of pain and muscles resistance. The orthopaedic surgeon manipulates the shoulder to bread free the adhesions. An intensive regime of physical therapy is required for a couple of weeks following MUA to prevent new adhesions from forming following the manipulation. MUA is contraindicated in patients who have a greater risk for fracturessuch as the elderly or those with osteoporosis, a patient with bleeding disorders and insulindependent diabetics.
In cases that are resistant to all other forms of the treatment orthopaedic surgery may be utilizedto remove the restrictive adhesions.



